What happens when your body won’t switch off survival mode?
For Kristy, a mother of three and former national swimmer, recovery from a mild COVID-19 infection turned into a relentless battle with exhaustion, unexplained symptoms, and a medical system that didn’t know what to do with her.
What followed was over a year of being housebound, living with what she now recognizes as POTS (Postural Orthostatic Tachycardia Syndrome) and long COVID—a combination that left her feeling like her nervous system had “completely malfunctioned.”
From Mild Infection to Systemic Collapse
When Kristy contracted COVID-19 over Christmas in 2022, she expected to bounce back quickly. The initial symptoms were manageable—just tiredness and a bit of pacing required to get through the day. But within months, things began to unravel.
“I was having good and bad days at first. But eventually, I crashed—and I never fully got back up.”
Over the next few months, Kristy found herself needing to lie down more often, struggling with waves of exhaustion. Then came the dizziness, heart palpitations, and strange nerve sensations. At one point, she called an ambulance, convinced she was having a heart attack.
But tests were inconclusive. Doctors sent her home with vague reassurances.
“They said everything looked fine. But I couldn’t walk across the room. I couldn’t sit upright without feeling crushed.”

Living With an Invisible Illness
By mid-2023, Kristy’s world had shrunk to the walls of her bedroom. She could no longer walk into her GP’s office without a wheelchair. Her muscles felt hollow. Neuropathy crept through her hands and feet. Her body trembled from simple movements.
“I’ve trained as an athlete. I’ve given birth. I know what pain and fatigue feel like. But this was different. It felt like my body was shutting down from the inside out.”
Specialists offered little more than pacing strategies. A long COVID clinic checked in monthly, but the support stopped after she completed an online presentation. There was no follow-up. No long-term care plan. No roadmap.
A New Path: Understanding the Nervous System
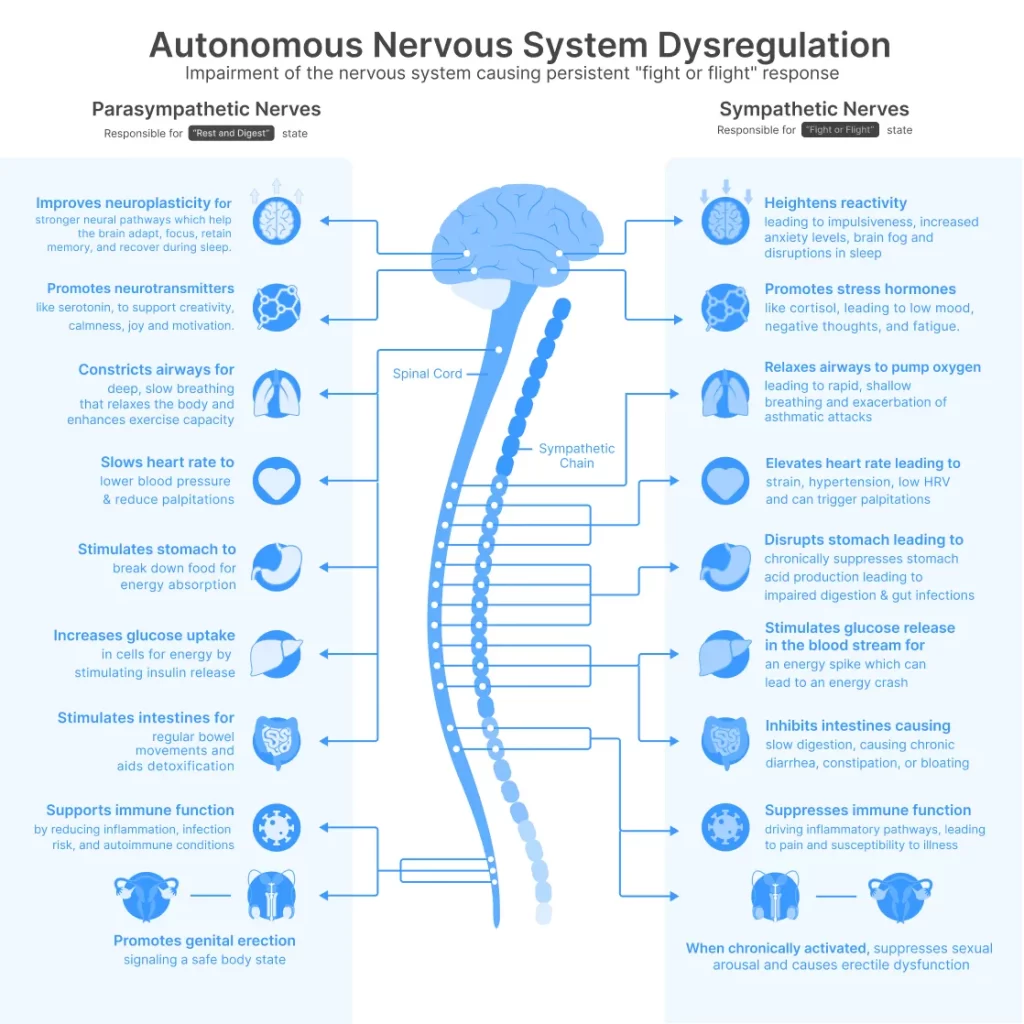
Desperate for answers, Kristy began researching the autonomic nervous system and came across emerging discussions around the vagus nerve—a key player in regulating heart rate, digestion, and inflammation.
“I kept reading about how the body can get stuck in fight-or-flight. And that if the vagus nerve isn’t working properly, you can’t shift into healing mode.”
The vagus nerve is the longest cranial nerve in the body, connecting the brain to vital organs including the heart, lungs, and gut. It acts like a brake on the body’s stress response, allowing you to move out of fight-or-flight and into rest-and-digest mode.
Research now shows that long COVID can disrupt the vagus nerve and throw the autonomic nervous system into chaos. A 2024 review in Frontiers in Neurology found that patients with long COVID often show signs of vagal dysregulation, contributing to symptoms like fatigue, tachycardia, nausea, and brain fog.
Dr. David Putrino, a neuroscientist at Mount Sinai Hospital, describes it this way: “When the vagus nerve is inflamed or misfiring, the body acts like it’s under constant threat. You can’t heal when you’re stuck in survival mode.”
What Kristy Tried Before
Like many patients, Kristy tried everything: pacing, breathwork, yoga nidra, dietary changes, and prescription medications. Some brought small relief. Others made her symptoms worse.
“I wasn’t looking for a miracle. I just wanted my body to feel safe again.”
Eventually, through her research, she discovered the concept of non-invasive vagus nerve stimulation (nVNS).

Small Steps Toward Stability
She learned that a branch of the vagus nerve runs through the ear, and that gentle electrical stimulation in this area—a method known as transcutaneous auricular VNS (taVNS)—could help restore autonomic balance.
She found a wearable device that had been studied at Imperial College London and NHS clinics, and began using it cautiously. The name: Nurosym.
“I started with five minutes, twice a day. Even that felt like a stretch. But after two weeks, I noticed my body calming down.”
Over time, she increased to 15 minutes, three times daily. The change was subtle but unmistakable.
“I could lift my arm. Walk to the bathroom. Eat sitting up. It felt like my body finally got the memo: you’re safe.”

How Nurosym Works
Nurosym uses gentle electrical pulses delivered via the tragus of the ear to activate the vagus nerve. The process is simple: moisten the ear clips, attach the device, and start a session.
Unlike vagus nerve “hacks” like cold plunges or breath holding, Nurosym provides consistent, controlled stimulation with clinically validated pulse parameters. It’s CE-marked as a medical device, and has been used in over 50 peer-reviewed trials.
The science is compelling:
- A 2024 randomized controlled trial (https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2024.1393371/full) showed a 35% reduction in anxiety, 19% improvement in sleep, and 45% improvement in fatigue after just two weeks of taVNS use.
- Another study (https://www.parasym.co/hrv.html) reported significant improvements in heart rate variability and autonomic regulation.
- A clinical review in Frontiers in Neurology found taVNS to be a promising tool in managing long COVID and chronic fatigue symptoms.
According to the device manufacturer, over 4 million sessions have been safely completed with zero serious adverse events.
Dr. Elias Quinton, a researcher at the Karolinska Institute, notes: “It’s one of the few neuromodulation devices with real-world safety and early efficacy data. We need more studies, but the results are promising.”
Nurosym is widely used in the medical community and recommended by thousands of healthcare professionals. It has also been adopted by high-performance organizations such as the national basketball team BC London Lions to support stress resilience and performance recovery.
“Nurosym is a device I use frequently in my practice as part of a holistic mind-body program that might include meditation, medication and alternative medicines where suitable,” says Dr. Gordon. “I find it works best for patients who have anxiety, as well as complex chronic conditions such as fibromyalgia, long COVID, chronic fatigue spectrum illness and in neurodivergent patients (who very often also suffer with anxiety).”
*Dr. Gordon has no financial relationship with Nurosym.

Building a New Baseline
Kristy now integrates VNS into her daily rhythm—during breathwork, rest, or simply while lying in bed. Her symptoms haven’t vanished, but her body no longer feels hijacked.
“It’s not magic. It’s not a quick fix. But it helps my body find the state where healing is even possible.”
She’s shared her experience with others in her support group. Even her husband uses the device occasionally for stress and tinnitus.

A Window of Hope
For those navigating long COVID, POTS, or other forms of nervous system dysregulation, Kristy’s story reflects a growing movement toward treating the nervous system as a core piece of chronic illness.
Devices like Nurosym are part of a new wave of medical technologies making VNS accessible to non-hospitalized patients. Studies suggest this method can improve heart rate variability, reduce inflammation, and enhance parasympathetic tone—all markers of a more resilient, responsive system.
As Dr. Kevin Tracey, a VNS pioneer, puts it: “Modulating the vagus nerve isn’t about hacking the body. It’s about returning it to balance.”
For Kristy, it marked the beginning of something she hadn’t felt in months: a sense of control.
“There’s no single cure. But there are ways to help your system shift out of chaos—and into something quieter, steadier. For me, that changed everything.”
Since the Nurosym device is quite an investment at €700 per piece, the company offers several programs to help patients access it:
- A 30-day money-back guarantee — try it for 30 days and return it if it doesn’t work for you
- VAT relief (UK only)
- Occasionally, the company runs remote research studies that offer subsidies for eligible participants
Learn more at nurosym.com



