When your body slips into constant “fight-or-flight” mode, you may notice an avalanche of symptoms—ranging from lingering fatigue and anxious thoughts to digestive woes and foggy thinking. At the center of it all is the vagus nerve: a crucial communication channel that helps regulate heart rate, digestion, mood, and immunity. If it’s impaired, even daily tasks can feel like a mountain to climb.
Find out if your vagus nerve might be contributing to your symptoms.
START VAGUS NERVE IMPAIRMENT ASSESSMENT
The Vagus Nerve & The Fight-or-Flight Response
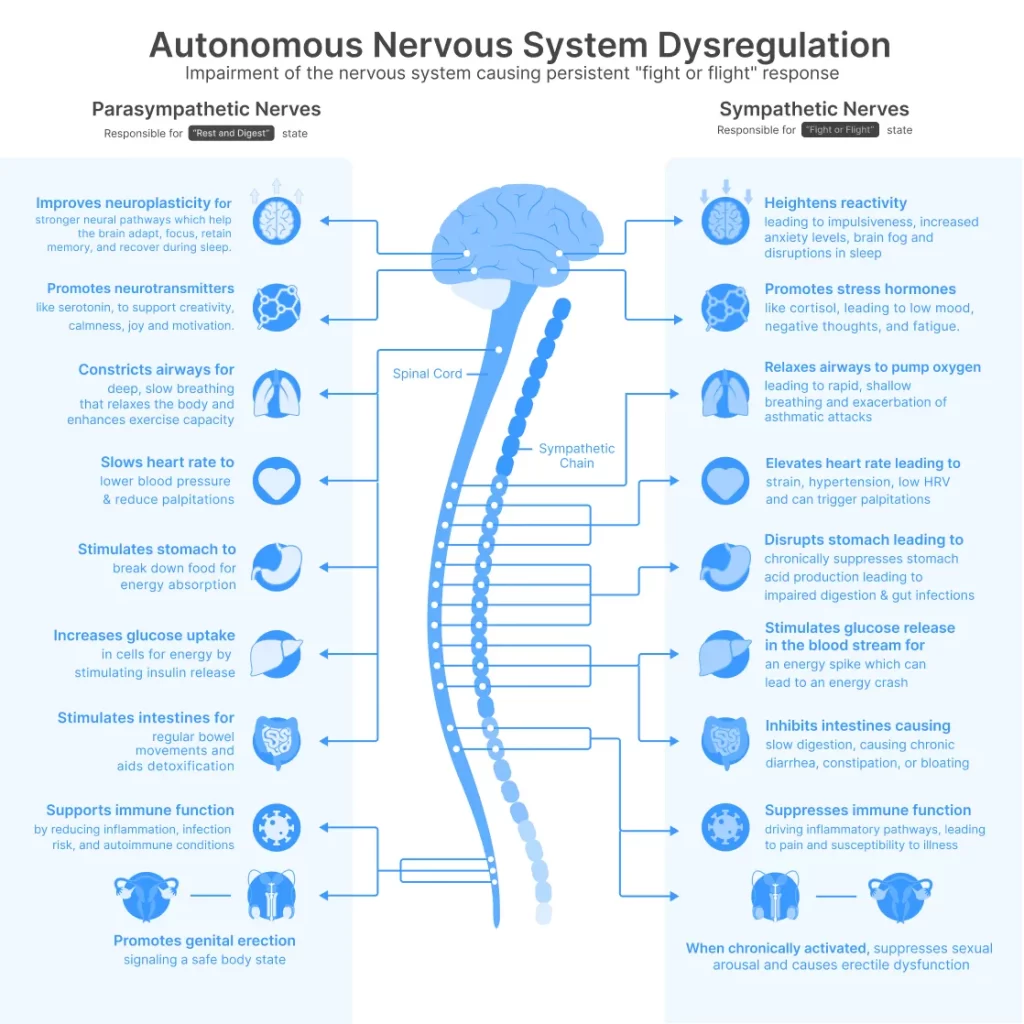
The vagus nerve is often called the body’s internal “reset button,” helping transition us from high-alert states back to rest and recovery. When it’s functioning optimally, your body can calm excess stress hormones, preserve steady digestion, and keep heart rhythms balanced. But when it’s compromised, you can become stuck in constant fight-or-flight, leading to symptoms such as elevated stress levels, jittery nerves, and poorer overall health [1].
Why Does This Matter?
Living in a constant state of physiological alarm strains multiple systems—your immune function can falter, your digestive system can slow, and feelings of anxiety may become more intense. Over time, such dysregulation can spiral into persistent fatigue, headaches, disrupted sleep, and more.
Conditions Linked to Vagus Nerve Impairment
Researchers have connected low vagal tone—a marker of vagus nerve health—to many chronic issues, including:
- Anxious thoughts, panic, or excessive stress [2]
- Persistent fatigue or low energy [5]
- Digestive complaints (acid reflux, bloating, constipation) [14]
- Brain fog and concentration difficulties
- Heart-related symptoms (palpitations, abnormal heart rate)
- Dizziness or trouble regulating blood pressure
- Mood swings, low mood, or mild depressive states
For many people, these problems appear unrelated at first. But scientific evidence suggests the vagus nerve may be the common denominator.
What Causes Vagus Nerve Impairment?

- Surgical Procedures: Unintended damage during neck or chest surgeries can disrupt nerve signals, causing swallowing difficulties or digestive slowdown [25].
- Autoimmune Conditions: Chronic immune attacks, such as those seen in Sjögren’s syndrome or lupus, may chip away at healthy nerve function over time [26].
- Toxins & Heavy Metals: Certain environmental agents (e.g., heavy metals or chemotherapy drugs) can negatively affect autonomic nerve fibers, including the vagus nerve [27].
- Diabetes & Metabolic Disorders: Persistently high blood sugars have been linked to nerve damage that can impact digestion and cardiovascular stability.
- Prolonged Stress or Trauma: Whether physical or psychological, chronic stress can reduce overall vagal tone, locking the body into a fight-or-flight loop.
From Invasive Surgery to Non-Invasive Solutions
In the early days, vagus nerve stimulation (VNS) required a surgical implant to treat conditions like severe epilepsy or hard-to-manage depression—effective but often a last resort due to high risks [9]. Thanks to ongoing research and technological breakthroughs, it’s now possible to stimulate the vagus nerve safely from the ear without an implant.
The Nurosym Difference
After a decade of research and over $10 million invested, Parasym developed Nurosym: a clinically validated, wearable device improving access to vagus nerve stimulation. Unlike its surgical predecessors, Nurosym’s transcutaneous vagus nerve stimulation (tVNS) approach avoids surgery, is easy to use at home, and taps into the same neural pathways.
How Vagus Nerve Stimulation Supports Better Health

Below are highlights from scientific studies—covering general auricular VNS and tVNS research—that reflect the potential effects of devices like Nurosym:
- Reduced Fatigue & Improved Mood
In studies on transcutaneous VNS, users reported notable drops in fatigue scores and quicker improvements on mood-assessment scales [31]. By supporting healthy autonomic balance, these therapies may help break the cycle of chronic tiredness. - Strong Heart Rate Variability (HRV)
HRV is a key indicator of resilience in your nervous system. Research on tragus stimulation shows a measurable rise in HRV, signaling better recovery from stress [32]. Higher HRV correlates with balanced “rest-and-digest” responses. - Relief in Postural Tachycardia (POTS)
People suffering from POTS experience racing heart rates upon standing. Randomized trials found that noninvasive VNS significantly reduced abnormal heart-rate spikes, aiding more stable blood flow [33]. - Lower Inflammation (TNF-α, IL-8)
VNS has demonstrated reductions in pro-inflammatory cytokines, including TNF-α and IL-8, which are often elevated in chronic health conditions [34]. This effect may contribute to reduced aches, better gut health, and improved overall wellness. - Cognitive & Memory Enhancements
Multiple investigations show that auricular VNS can improve certain memory tasks and cognition in both older adults and individuals with brain fog [36],[37]. By boosting parasympathetic tone, the brain may achieve better focus and processing speed.
Taking the Next Step: Get Your Nervous System Score
Feel like you’ve tried everything—supplements, changes in diet, better sleep routines—yet still battle stress, fatigue, or nagging gut issues?
A quick assessment can be the very first step to illuminating whether vagus nerve impairment is part of the puzzle. Our easy questionnaire, developed from peer-reviewed research, can help reveal whether you’re showing red flags of low vagal tone.
The Promise of Nurosym
Exploring safe, non-invasive vagus nerve stimulation is a leap forward in modern medicine. Nurosym’s wearable design focuses on:
- Simplicity: Convenient daily sessions, no special facilities or surgeries required.
- Clinical Evidence: Backed by multiple studies on tVNS, showing improved energy, reduced stress, and better cognitive performance.
- In-Home Comfort: A user-friendly approach you can incorporate into your existing routine.
Final Thoughts
Your vagus nerve, often overlooked, may hold the key to more stable energy levels, calmer moods, and resilient digestion. Rather than letting your body remain in a fight-or-flight spiral, you can seek ways to restore balance—and modern neuromodulation technology can help.
Ready to take charge of your nervous system health? Start by taking our short assessment:
The article does not in any way constitute as medical advice. Please seek consultation with a licensed medical professional before starting any treatment. This website may receive commissions from the links or products mentioned in this article.
References
(1) Yuan, H., & Silberstein, S. D. (2016). Vagus Nerve and Vagus Nerve Stimulation: A Comprehensive Review. Headache, 56(2), 287–296. https://pubmed.ncbi.nlm.nih.gov/26364692/
(2) George, M. S., et al. (2008). A Pilot Study of Vagus Nerve Stimulation for Treatment-Resistant Anxiety Disorders. CNS Spectrums, 13(11), 953–963. https://pubmed.ncbi.nlm.nih.gov/20633378/
(5) Laborde, S., et al. (2021). Enhanced Cardiac Vagal Tone in Mental Fatigue: A Heart Rate Variability Study. Frontiers in Neuroscience, 15, 612623. https://pubmed.ncbi.nlm.nih.gov/34381453/
(14) Bonaz, B., et al. (2024). Enteric Neuropathy and the Vagus Nerve: Therapeutic Implications. Neurogastroenterology & Motility, 36(3), e14722. https://pubmed.ncbi.nlm.nih.gov/38873822/
(25) Lee, J., et al. (2011). Unilateral High Vagal Paralysis: Relationship of Severity to Feeding Tube Dependency. Laryngoscope, 121(3), 571–576. https://pubmed.ncbi.nlm.nih.gov/21271569/
(26) Davies, K., & Ng, W. F. (2021). Autonomic Nervous System Dysfunction in Primary Sjögren’s Syndrome. Frontiers in Immunology, 12, 702505. https://pubmed.ncbi.nlm.nih.gov/34381453/
(27) Hershkovich, H., et al. (2013). Associations Between Autonomic Dysfunction and Pain in Chemotherapy-Induced Polyneuropathy. European Journal of Pain, 17(9), 1347–1355. https://pubmed.ncbi.nlm.nih.gov/23776126/
(31) Fry, W., et al. (2022). Auricular Vagus Nerve Stimulation for Chronic Fatigue. Journal of Clinical Medicine, 11(9), 2633. https://pubmed.ncbi.nlm.nih.gov/35512986/
(32) Bretherton, B., et al. (2021). Transcutaneous Auricular Vagus Nerve Stimulation and Heart Rate Variability: A Parameter Optimization Study. Brain Stimulation, 14(6), 1357–1367. https://pubmed.ncbi.nlm.nih.gov/34662844/
(33) Chen, L., et al. (2024). Noninvasive Vagus Nerve Stimulation in Postural Tachycardia Syndrome: A Randomized Controlled Trial. Journal of the American College of Cardiology, 83(12), 1123–1135. https://pubmed.ncbi.nlm.nih.gov/37999672/
(34) De Herdt, V., et al. (2009). Effects of Vagus Nerve Stimulation on Pro- and Anti-Inflammatory Cytokine Induction in Patients with Refractory Epilepsy. Journal of Neuroinflammation, 6, 21. https://hmlfunctionalcare.com/wp-content/uploads/2021/06/Effects-of-vagus-nerve-stimulation-on-pro-and-anti-inflammatory-cytokine-induction-in-patients-with-refractory-epilepsy.pdf
(36) Giraudier, M., et al. (2018). Transcutaneous Vagus Nerve Stimulation Boosts Associative Memory in Older Adults. Neurobiology of Aging, 72, 146–154. https://pubmed.ncbi.nlm.nih.gov/25805212/
(37) McIntire, L. K., et al. (2021). Cervical Transcutaneous Vagal Nerve Stimulation Improves Cognitive Performance During Sustained Wakefulness. Sleep, 44(10), zsab152. https://pubmed.ncbi.nlm.nih.gov/34112935/



