Introduction: The Vagus Nerve – The Superhighway of the Nervous System
The vagus nerve (cranial nerve X) is the longest nerve of the autonomic nervous system and a key part of the parasympathetic “rest and digest” network. It extends from the brainstem down through the neck and into the chest and abdomen, connecting to the heart, lungs, gut, and other organs 1. Often called the body’s information superhighway, it carries signals that help regulate heart rate, digestion, and even immune responses via the cholinergic anti-inflammatory pathway 2,1. In recent years, vagal tone – a measure of vagus nerve activity – has garnered growing interest in both scientific research and wellness communities. This surge in interest is fueled in part by Stephen Porges’ Polyvagal Theory, which links vagal activity to emotional regulation and social connection 3. Indeed, polyvagal theory has become popular among some clinicians and patients for its explanation of how vagus nerve dynamics relate to stress, safety, and even trauma recovery 3. Concurrently, researchers like Kevin Tracey have illuminated the vagus nerve’s crucial role in controlling inflammation, coining the term “inflammatory reflex” to describe how vagal signals can rapidly curb immune responses 2. These insights have spurred interest in vagus nerve stimulation (VNS) as a therapeutic strategy. Traditionally, VNS meant an implanted device, but today there is growing enthusiasm for non-invasive approaches to stimulate the vagus nerve and improve “vagal tone.” In this article, we will explore the anatomy and functions of the vagus nerve, what can go wrong when this system is out of balance, and evidence-based methods – from breathing exercises to advanced devices – to therapeutically stimulate the vagus nerve.
Anatomy of the Vagus Nerve: Pathways Through the Body
The vagus nerve originates in the medulla oblongata of the brainstem and meanders (“vagus” is Latin for wandering) through the body, with branches that innervate the throat, heart, lungs, and digestive tract 1. There are actually two vagus nerves (left and right), which together carry both sensory (afferent) signals from organs to the brain and motor (efferent) signals from the brain to organs. As the vagus travels downward, it interweaves with other nerves and gives off branches, such as the cardiac branches to the heart and pulmonary branches to the lungs 4. In the abdomen it forms networks (plexuses) that influence the stomach, intestines, liver, and other organs 4. This broad reach enables the vagus to act as a master regulator of internal organ function and homeostasis.
Notably, the vagus also has a small auricular branch that reaches the skin of the outer ear – specifically parts of the ear canal and auricle (outer ear) 5. In fact, anatomical research shows that this auricular branch of the vagus nerve (ABVN) is essentially the only branch of the vagus that comes to the body’s surface 6. This means the outer ear is a unique gateway to directly access the vagus nerve without invasive procedures. The ABVN (sometimes called Arnold’s nerve) supplies sensory fibers to areas like the tragus and cymba conchae of the ear 5. Stimulating this area (for example with electrode clips or earpiece devices) can activate vagal pathways, as confirmed by neuroimaging evidence 7,8. From an anatomical standpoint, this little nerve branch has outsized importance: it provides a convenient entry point for therapeutic VNS – a fact that has driven the development of transcutaneous auricular VNS (taVNS) methods, which we will discuss later.
Key Functions of the Vagus Nerve
The vagus nerve’s extensive reach translates to a diverse array of physiological functions. Broadly, the vagus helps maintain homeostasis – the body’s internal equilibrium. Via its efferent (motor) fibers, the vagus exerts a calming influence on target organs: slowing the heart rate, stimulating digestive processes, and promoting restfulness. For example, vagal input to the heart’s pacemaker slows the sinus rate, which is why high vagal tone is associated with a lower resting heart rate and greater heart rate variability (a marker of cardiovascular health) 9. Vagal signals to the gut stimulate peristalsis and secretion, supporting efficient digestion. Importantly, the vagus is also a key component of the antistress response. Vagal activation can counteract the “fight or flight” effects of the sympathetic nervous system, producing a relaxation response (hence deep breathing or meditation, which increase vagal activity, tend to induce calm).

In addition, the vagus nerve is the sensory backbone of the so-called “gut-brain axis.” Up to 80% of vagal fibers are afferent, carrying information from internal organs back to the brain 1. These signals inform the brain about the state of the body – everything from blood pressure and gut nutrient content to the presence of inflammation. Based on this sensory input, vagal reflex pathways help regulate inflammation and immunity. In 2002, Tracey and colleagues demonstrated that vagus nerve stimulation can suppress pro-inflammatory cytokine release during systemic inflammation, coining the concept of a cholinergic anti-inflammatory reflex 2. The vagus achieves this via a pathway in which vagal efferents release acetylcholine that acts on immune cells (e.g. macrophages) to dampen inflammatory cytokine production 1. This “hard-wired” neural control of immunity is an elegant mechanism by which the nervous system can quickly curb excessive inflammation – essentially a brake on the immune system to prevent damage from overreacting 2.
The vagus nerve also influences neurotransmitter systems and brain function. Vagal afferents project to the nucleus tractus solitarius (NTS) in the brainstem, which in turn connects to regions that regulate mood and arousal (such as the locus coeruleus and dorsal raphe nucleus). Stimulation of vagal pathways has been shown to activate the cholinergic system in the brain involved in learning and memory 10. In fact, researchers have observed that vagus nerve stimulation can enhance memory consolidation and cognitive performance, presumably by boosting neuromodulators like acetylcholine and norepinephrine in key brain circuits 11,10. This underlies the interest in vagal stimulation for conditions like Alzheimer’s disease and depression. Clinically, implanted VNS therapy (described more below) was found to improve mood in some patients, leading to its approval as an adjunctive treatment for refractory depression in 2005 12. The vagus’ role in mental health is an area of intense research: low vagal tone has been linked with anxiety and mood disorders, while interventions that increase vagal activity (from deep breathing exercises to VNS devices) often correlate with reductions in anxiety and improvements in emotional resilience 13,14. In summary, the vagus nerve is a critical bi-directional communication highway between brain and body, regulating visceral organ function, immune responses, and even aspects of brain chemistry that affect our mental state 1,15.
Autonomic Nervous System Imbalance: When Fight, Flight, or Freeze Takes Over
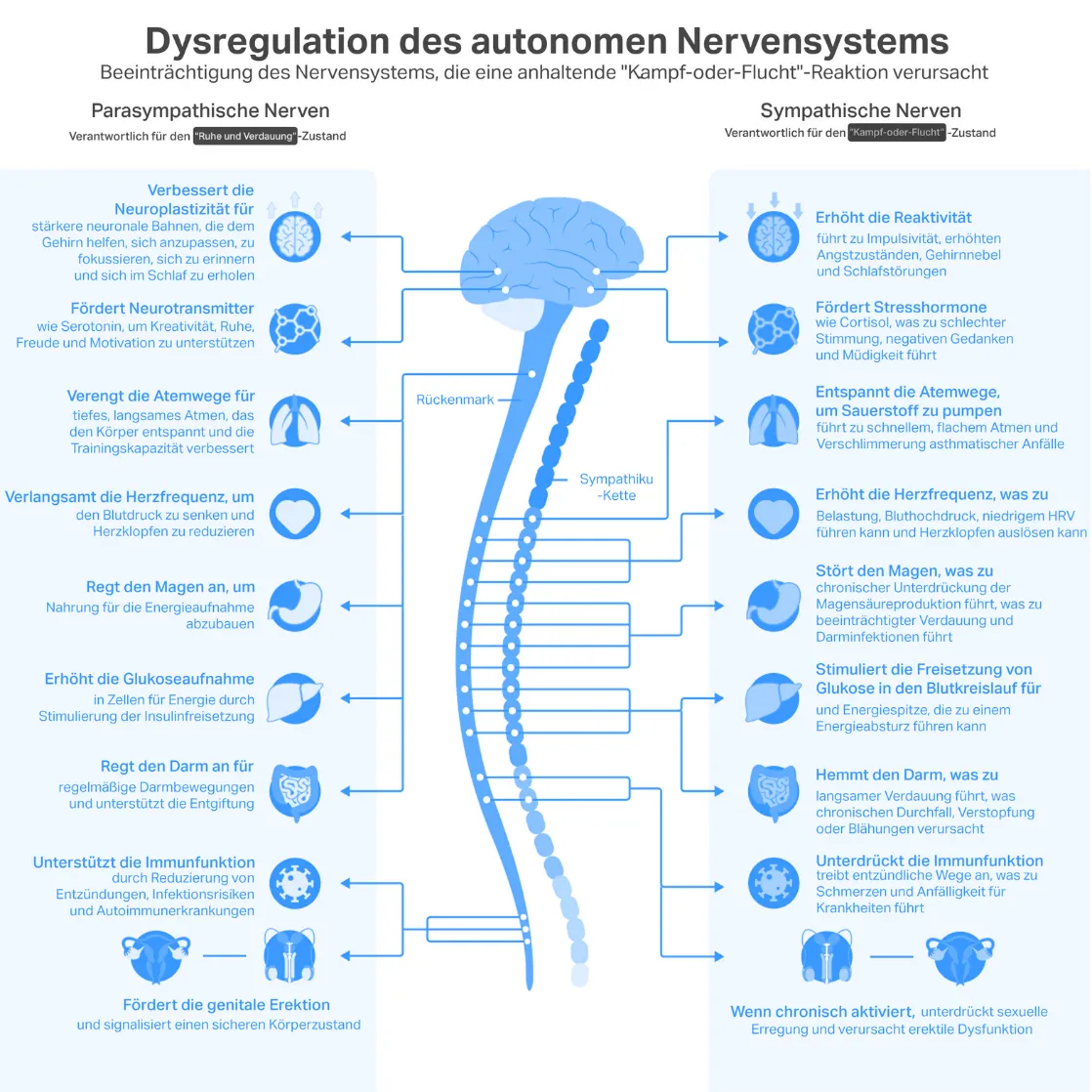
The autonomic nervous system has two primary divisions: the sympathetic (“fight or flight”) and the parasympathetic (“rest and digest”). Under normal conditions, these systems dynamically balance each other. The vagus nerve, as the main parasympathetic conduit, applies a braking effect on the heart and other organs, promoting calm states (sometimes termed the “vagal brake”). However, chronic stress can tip the scales toward sympathetic dominance, overwhelming the vagal brake. In a state of sustained fight-or-flight activation, stress hormones stay elevated, heart rate and blood pressure remain high, and digestion and sleep are disrupted. Over time, this autonomic imbalance contributes to anxiety, insomnia, hypertension, and metabolic issues. Research in psychophysiology has shown that inadequate vagal activity (low vagal tone) is associated with poorer emotion regulation and greater stress reactivity 13. Thayer and Lane’s neurovisceral integration model posits that a well-functioning vagus is crucial for inhibiting the excessive firing of stress circuits; if this inhibitory vagal tone is lacking, stress responses can spiral (a positive feedback loop), contributing to anxiety and mood dysregulation 13.
Beyond fight or flight, the vagus is also implicated in the “freeze” response – an extreme defensive state of immobilization. Polyvagal Theory differentiates the vagal pathways into two branches: a ventral vagal system associated with safe social engagement, and a dorsal vagal system that, when triggered in life-threatening situations, can produce a freeze or shutdown state (akin to an animal playing dead) 16. This dorsal vagal response can manifest as fainting or extreme conservation of energy and is thought to underlie the “collapse” or dissociative response some people have under trauma. In modern life, chronic stimuli (like relentless stress or past trauma) may inappropriately evoke aspects of this shutdown response, leading to symptoms such as fatigue, low blood pressure, or emotional numbness. Porges and others have suggested that some cases of depression or chronic fatigue involve a dysregulated dorsal vagal state – essentially an overshooting of the parasympathetic response into an immobilization mode. Overall, whether it’s sympathetic overdrive or maladaptive vagal freezing, autonomic imbalance can wreak havoc on physical and mental health. Many therapeutic approaches (from heart rate variability biofeedback to yoga) explicitly aim to restore vagal-sympathetic balance, quieting the fight/flight response while preventing excessive freeze responses.
Causes of Vagus Nerve Dysfunction
What can cause the vagus nerve to malfunction or its tone to be diminished? Researchers are still unraveling the causes, but several factors have been implicated:
- Chronic stress: Persistent psychological or physical stress can suppress vagal activity and lead to low vagal tone over time 13. Emotional stress is linked to reduced heart rate variability (an indicator of vagal function) and can alter the sensitivity of vagal reflexes. Essentially, the vagal brake becomes less responsive under chronic stress, as the sympathetic system predominates.
- Inflammation and Infection: Systemic inflammation can interfere with vagal signaling. The vagus nerve helps sense and modulate inflammation, but if inflammatory cytokines are constantly elevated, it may blunt vagal feedback loops. Notably, certain infections can trigger vagus-related dysfunction. For example, infection with Epstein–Barr virus (EBV) – especially if reactivated later (as has been observed in some long COVID patients – has been hypothesized to impair vagal pathways and contribute to chronic symptoms 17. In animal studies, inflammatory molecules like interleukin-1 can activate vagal afferents and induce “sickness behavior” (fatigue, malaise, reduced appetite), and cutting the vagus nerve prevents many of these sickness symptoms 18,19. This suggests that excessive immune activation (e.g. during severe infection or autoimmune conditions) might alter vagal nerve function or responsiveness. Patients with disorders like rheumatoid arthritis or inflammatory bowel disease often show reduced vagal tone, and boosting vagal activity (even via implanted VNS) has been explored to counter inflammation 2,1.
- Viral neuropathies: Some viruses can directly affect the vagus nerve. For instance, there is speculation that SARS-CoV-2 (the virus causing COVID-19) might damage vagal sensory fibers or nuclei in some patients, given the vagus’s involvement in regulating lung, heart, and gut function (which are often disrupted in long COVID). EBV reactivation, as noted, might also damage or inflame vagal pathways 17.
- Neurodegenerative diseases: Conditions like diabetes (which can cause peripheral neuropathy) or neurodegenerative disorders can impair autonomic nerves including the vagus. Parkinson’s disease, for example, is associated with early vagal dysfunction (some researchers even hypothesize that PD pathology might spread from the gut to the brain via the vagus nerve). Alzheimer’s disease patients often have blunted parasympathetic activity. In a mouse model of Alzheimer’s, stimulating the vagus shifted microglia (brain immune cells) from a proinflammatory to a neuroprotective state 20,21, hinting that vagal dysfunction could exacerbate neuroinflammation in such disorders. Conversely, vagus nerve stimulation is being studied as a way to improve cognitive function in early Alzheimer’s 20,21.
- Poor sleep: Sleep and vagal tone are tightly linked. Deep, restorative sleep naturally boosts vagal activity (evidenced by slower heart rate and high heart rate variability at night). Chronic insomnia or sleep apnea can lower baseline vagal tone. In turn, low vagal tone may contribute to sleep problems – a vicious cycle.
- Gut issues and diet: Since the vagus monitors gut status, chronic gastrointestinal problems might strain vagal pathways. For example, longstanding dysbiosis or infection in the gut could lead to continuous vagal afferent firing (signaling distress), potentially desensitizing the nerve over time. Nutrient deficiencies (like B vitamins) that affect nerve health could also play a role in vagal neuropathy
It’s worth noting that measuring vagus nerve “dysfunction” is challenging – clinicians often rely on proxies like heart rate variability or tests of reflexes (e.g. gag reflex, which the vagus mediates). Nonetheless, when the vagus is underperforming, the consequences – from increased inflammation to anxiety – can be far-reaching. This is why interventions that can restore healthy vagal tone are of such great interest.
History and Evolution of Vagus Nerve Stimulation (VNS)
Using electricity to stimulate the vagus nerve has an intriguing history. The first attempts date back to the 19th century, when scientists experimented with stimulating the carotid region (where the vagus travels) to treat epilepsy 22. Those early forays were not very successful, but they planted the seed for vagus nerve stimulation as a therapy. Fast forward to the late 20th century: after promising animal studies, an implantable VNS device was developed for human use. In 1997, the FDA approved VNS therapy for refractory epilepsy – patients with seizures not controlled by medication. This implanted device, roughly the size of a stopwatch, is surgically placed in the chest with a wire coiled around the left vagus nerve in the neck. It delivers intermittent electrical pulses to the vagus. Epilepsy trials showed that VNS could significantly reduce seizure frequency in some patients, albeit with variable responses. Subsequently, in 2005, VNS was also approved for treatment-resistant depression 12 after clinical studies found that some patients’ mood improved with vagal stimulation.
Implantable VNS provided a new lifeline for certain patients, but it has drawbacks. Surgery is required to implant the device and coil, carrying risks of infection or nerve damage (albeit low). Furthermore, stimulation of the vagus in the neck can produce side effects like coughing, throat pain, or hoarseness of voice due to the current spreading to laryngeal nerves 23. One significant side effect is a change in voice or mild vocal cord paralysis – patients often report their voice gets raspy during stimulation 23. Other common side effects include neck discomfort, coughing, or shortness of breath during a stimulation pulse 23. Despite these issues, over 100,000 implantable VNS devices have been implanted worldwide for epilepsy and depression. Long-term studies suggest that some patients continue to experience benefits (seizure reduction, mood stabilization) with chronic VNS, and the device can be adjusted or turned off externally by a magnet if needed.
The success of implanted VNS – and its limitations – led to a shift toward less invasive approaches. Around the 2010s, researchers began exploring transcutaneous VNS, stimulating the vagus from outside the body. Two main routes were tried: the cervical vagus (through the skin of the neck) and the auricular branch (on the ear). Stimulating the cervical vagus with surface electrodes on the neck (as in some headache devices) can activate vagal fibers, but the ear approach (taVNS) gained particular interest because of the ABVN’s accessible location. Crucially, non-invasive VNS (often called nVNS) was found to have a much lower risk profile – no surgery, and side effects (like mild skin irritation or tingling) were minor in comparison 24. By the mid-2010s, the first portable auricular VNS stimulators were being tested in clinical trials for a range of conditions: epilepsy, migraine, depression, tinnitus, and more 22. Early results have been encouraging, leading some researchers to conclude that non-invasive VNS, while perhaps a bit less potent than the implanted kind, “exhibits greater safety” and may achieve similar physiological effects in some applications 24. In Europe, several transcutaneous VNS devices earned CE-mark approval in the pain and psychiatric domains, and in 2018 the FDA approved an external vagus stimulator for treating cluster headaches. We’re now in an era where VNS is not only an implanted neuromodulation therapy but also a handheld, at-home intervention for potentially modulating stress responses, inflammation, and more.
Auricular VNS: Why the Ear Is a Game Changer

Stimulating the vagus via the ear has opened a new chapter in neuromodulation. The auricular branch of the vagus nerve (ABVN) makes this possible – as noted earlier, it provides a gateway to influence vagal pathways simply by applying electrodes to specific points on the outer ear. The cymba conchae (a region of the ear’s conchal bowl) and the tragus are two spots with vagal innervation that are commonly targeted. From a practical standpoint, auricular VNS has several advantages over traditional (neck) VNS:
- Non-invasive and safer: There is no need for surgery or implantation. A small electrode ear-clip or an earbud-like device can deliver the stimulation. This eliminates surgical risks and vastly reduces side effects. Patients using auricular VNS occasionally report tingling or slight discomfort on the ear, but it lacks the coughing or voice changes seen with cervical VNS implants because the stimulation is more localized and gentler. A recent systematic review confirmed that taVNS is generally safe and well-tolerated, with mostly mild, transient effects 25.
- Self-administered and convenient: Auricular VNS devices can be used at home, by the patient themselves. Typically, a device will clip onto the ear and attach to a small stimulator (about the size of a phone or smaller). Sessions can be done daily. This puts treatment in the patient’s hands (with guidance from a clinician), rather than requiring in-hospital procedures. The ease of self-administration means patients can integrate vagus stimulation into their daily routine – much like doing a workout for the nervous system.
- Accessible branch = daily dosing: Because the ear is so accessible, patients can receive frequent stimulation without risk. Implanted VNS is often programmed to cycle on for 30 seconds every 5 minutes all day, which is effective but if any adverse effect occurs, you must turn it off. With ear VNS, patients can do, say, two or three 15-minute sessions per day as needed. The ability to easily “dose” the vagus nerve regularly may be key for chronic conditions (similar to how daily medications are needed to manage blood pressure or diabetes).
- Targeted stimulation: Interestingly, evidence from fMRI studies shows that stimulating the ABVN in the left ear activates similar brainstem and cortical regions as stimulating the cervical vagus 7,8. This indicates that auricular VNS is engaging central vagal circuits. Some studies even suggest certain ear locations might preferentially activate specific pathways – for instance, cymba conchae vs tragus stimulation could have slightly different effects on heart rate or brain activation 26. Ongoing research is examining the optimal ear targets and stimulus parameters for various therapeutic goals (e.g., reducing pain versus reducing anxiety).
- No interference with the neck or heart: Auricular VNS avoids direct stimulation of fibers near the cardiac branch (the reason implanted VNS is usually on the left side is to minimize affecting heart rhythm). Thus, auricular stimulation has not been observed to cause significant bradycardia or other cardiac side effects – an important safety consideration. Of course, anyone with a pacemaker or serious heart condition should only use these devices under medical supervision, but overall the ear route appears intrinsically safer for the heart.
The bottom line is that auricular VNS offers a relatively risk-free way to tap into the vagus nerve’s broad healing potential. It has democratized VNS therapy – what was once only available via neurosurgery can now be achieved with a wearable device. Given these benefits, it’s no surprise that interest in taVNS has exploded in the last decade. From academic labs to start-up companies, many are now working on optimizing ear-based vagus nerve stimulators. In the next sections, we’ll look at both low-tech und hightech methods to activate the vagus nerve, and the evidence behind them.
Popular Vagus Nerve Activation Techniques (DIY Approaches)
Long before electronic vagus nerve stimulators existed, people intuitively discovered ways to influence the vagus nerve through various practices. Many traditional relaxation techniques and wellness habits happen to stimulate vagal pathways. Here we compare some popular do-it-yourself vagus nerve activation techniques – their proposed mechanisms, evidence, and pros/cons:
| Technique | Proposed Mechanism | Evidence of Efficacy | Pros | Cons |
| Deep Breathing | Slow, diaphragmatic breathing increases vagal tone by activating stretch receptors in the lungs and triggering vagal reflexes 9. Extending the exhale phase is especially vagusstimulating. | Shown to reduce heart rate and blood pressure. Jerath et al. (2006) hypothesized that slow pranayama breathing “resets” the autonomic system toward parasympathetic dominance 9,27. Clinical studies link paced breathing to improved heart rate variability and reduced anxiety. | Easy, free, and accessible anywhere. Can produce immediate calming. Also improves focus and oxygenation. | Requires practice for maximal benefit (beginners may not breathe deeply enough). Effects are temporary unless done regularly. Severe anxiety may make slow breathing difficult initially. |
| Humming / Chanting | Gentle vocalization (e.g. humming “OM” or singing) causes vibrations in the vocal cords and middle ear that may stimulate the auricular branch of the vagus 28. Exhaling slowly while humming also engages the diaphragm and vagal breathing reflex. | Brain imaging during “OM” chanting shows deactivation of limbic brain regions associated with stress, consistent with increased vagal input to the brain 28. Anecdotally, many report that humming or singing calms them – likely via vagal modulation of heart rhythm. Some therapists incorporate gargling or chanting as vagal exercises (though formal trials are limited). | Simple and soothing; can be done discreetly (humming) or in groups (chanting, singing). No equipment needed. Also improves respiratory and vocal cord control. | Limited direct clinical research specific to vagal tone. Effects may vary – not everyone finds humming relaxing. Loud chanting not always feasible in daily life. Those with hearing issues may get less vibratory stimulation benefit. |
| Cold Exposure (Diving Reflex) | Splashing the face or neck with cold water (or full-body cold showers) triggers the mammalian diving reflex, which via the vagus nerve dramatically slows heart rate and shunts blood to core organs 29,30. This reflex, mediated by vagal pathways, is meant to conserve oxygen – and has a side effect of inducing calm | Even without breathholding, facial cold exposure increases high-frequency heart rate variability, indicating increased vagal activation 31,32. Many people report that an icy face dunk or cold shower “resets” their mood and reduces acute anxiety – likely by vagally-induced slowing of the heart and a surge of endorphins. UVA researchers confirm that the cold-water face dunk can rapidly decrease heart rate and anxiety, thanks to vagus nerve fibers signaling the brain to trigger the parasympathetic dive response 29,33. | Quick acting – relief can occur within seconds or minutes. No special tools needed (just cold water). Can be very useful during panic attacks or acute stress to induce a physiological calm via the vagus. | The shock of cold is uncomfortable for many. Not suitable if you have certain heart conditions (a sudden vagalinduced slow heart rate can cause dizziness). Effects are shortterm (a quick calm, not a lasting solution for chronic stress). Also, not everyone can or should do full cold immersions – start gently (cool water on face). |
| Meditation & Yoga | Mindfulness meditation and yoga practices incorporate slow breathing, posture, and mental focus that collectively enhance vagal activity. Meditation often increases the rest-and-digest state by quieting the sympathetic drive. Yoga, especially styles emphasizing pranayama (breath control) and relaxation, stimulates the vagus through breathing and perhaps direct stretches of vagal nerve pathways in the neck/chest. | Numerous studies link mind–body practices to higher vagal tone. For example, mindfulness training has been associated with improvements in heart rate variability and stress resilience 14. Tang et al. (2015) reviewed how meditation can remodel brain circuits and improve autonomic regulation. Certain yoga poses (like inversions) also activate baroreceptors and vagal reflexes. While individual results vary, overall the evidence suggests regular meditation/ yoga shifts the nervous system toward parasympathetic dominance (lowering heart rate, blood pressure, and cortisol). | Well-studied and with broad health benefits beyond vagal tone (improved mood, concentration, flexibility, etc.). Can be tailored to individual abilities (meditation is accessible even to those with limited mobility). Effects can be long-lasting with habitual practice – essentially “training” your nervous system. | Requires time, consistency, and learning proper techniques. Some may find it difficult to sit still and meditate initially (ironically those with low vagal tone may feel restless). Yoga carries a minor risk of injury if done improperly. It may take weeks to months of practice to see significant objective changes in vagal tone. |
Each of these DIY methods taps into the vagus nerve in its own way. They are generally low-risk and can be combined (e.g. a yoga session that includes deep breathing and chanting “OM” covers three methods!). It’s important to note that while these techniques have promising evidence and make intuitive sense, individual responses differ. Some people might respond dramatically to breathing exercises, while others find meditation more effective. These self-regulation tools are best seen as part of a holistic approach to tone the vagus nerve and balance the autonomic nervous system.
Scientific Evidence on Auricular VNS

Moving from home techniques to high-tech devices, what does research show about auricular VNS (aVNS) in clinical contexts? Over the past decade, aVNS has been tested in a wide range of pilot studies and clinical trials. Here is a snapshot of findings across various domains:
- Psychische Gesundheit: Several studies suggest aVNS can improve symptoms of anxiety and depression. For instance, an open-label trial of transcutaneous VNS in patients with major depressive disorder with peripartum onset (postpartum depression) found significantly reduced depression scores over 6 weeks of daily at-home stimulation 34,35. By the trial’s end, 74% of participants had a clinically significant response and over 60% went into remission 36,37– notably high rates for a hard-to-treat condition (though without a placebo control, more research is needed). In generalized anxiety disorder, small studies have reported reductions in anxiety levels with daily auricular VNS use compared to sham. Patients often report feeling calmer and sleeping better after a few weeks of aVNS. Neuroimaging studies give insight into why: aVNS can increase activity in brain regions that regulate mood and decrease reactivity of stress circuits 8,11. There is also early evidence that aVNS may help PTSD symptoms, by promoting a physiological state of safety that could complement psychotherapy.
- Cognitive Function: One of the most intriguing findings comes from cognitive neuroscience. In 2015, Jacobs et al. demonstrated that a single session of auricular VNS significantly boosted associative memory performance in healthy older adults 38,39. In their randomized crossover study, participants were better at remembering face–name pairs when receiving mild tragus stimulation versus sham 38,39. This suggests that aVNS can enhance memory encoding, likely by activating neuromodulatory systems in the brain (as discussed, vagal activation can increase acetylcholine and norepinephrine release, which aid memory). This finding has spurred interest in aVNS as a potential therapy for early Alzheimer’s disease or mild cognitive impairment. Trials are underway to see if repeated aVNS might slow cognitive decline or improve attention and memory in patients. Even in healthy individuals, researchers (including at Maastricht University) have explored aVNS for brain training – for example, examining whether stimulating the ear during learning tasks can improve neuroplasticity. So far, results are mixed but promising: one group found enhanced memory and alertness in volunteers using aVNS compared to sham 38,40.
- Cardiovascular and Inflammatory Effects: Since the vagus nerve controls heart rate and inflammation, it makes sense to examine those outcomes. Short-term aVNS has been shown to modulate heart rate variability (HRV) – an indicator of vagal cardiac control. In a controlled experiment, Badran et al. noted that certain stimulation parameters (e.g. 10 Hz pulses) delivered to the tragus could acutely increase HRV and even slightly reduce heart rate in healthy adults 26,41. This cardiac-vagal engagement is modest but suggests that aVNS might benefit conditions like heart failure or arrhythmias where increasing vagal tone is desirable. On the inflammatory front, aVNS has been tested in disorders like rheumatoid arthritis and inflammatory bowel disease. One pilot in patients with Crohn’s disease (using an ear clip stimulator daily) showed reduced C-reactive protein (a blood inflammation marker) and improved disease activity scores, hinting at an anti-inflammatory effect. A systematic review in 2021 noted that across studies, aVNS tends to lower levels of inflammatory cytokines like TNF-alpha and interleukin-6, although results vary and more large trials are needed 42,43. Excitingly, a small study in long COVID patients with fatigue found that four weeks of daily aVNS led to subjective improvements in fatigue and cognitive fog, and some normalization of inflammatory markers – possibly by reining in an overactive immune response.
- Gastrointestinal Disorders: Given the vagus’ crucial role in gut motility and secretion, investigators have tried aVNS for conditions such as gastroparesis (delayed stomach emptying), functional dyspepsia, and irritable bowel syndrome (IBS). A recent randomized trial in patients with functional dyspepsia showed that four weeks of auricular VNS (at either 10 Hz or 25 Hz) improved symptoms significantly more than sham stimulation 44. Patients reported less bloating, nausea, and stomach pain, and objective tests showed slightly improved gastric emptying. In IBS, especially the constipation-predominant type, studies have found that aVNS can relieve abdominal pain and improve bowel habits 45. For example, one trial in IBS-C patients found a 50% reduction in abdominal pain frequency and increases in weekly spontaneous bowel movements with daily aVNS versus sham over 8 weeks 45. The mechanism may involve vagal modulation of gut-brain signaling, reducing visceral hypersensitivity (the vagus telling the brain “all is calm in the gut”) and normalizing motility. Researchers at Maastricht University published findings suggesting aVNS can enhance communication between the gut and brain regions involved in reward and pain modulation 46. And in adolescents with IBS, a small study even observed beneficial changes in gut microbiome diversity after several weeks of auricular VNS 47.
Overall, the scientific evidence, while still emerging, paints a picture of broad therapeutic potential for transcutaneous auricular VNS. It is being explored in neurological disorders (epilepsy, migraine, stroke rehabilitation), psychiatric disorders (depression, anxiety, PTSD), cardio-metabolic conditions (POTS – postural orthostatic tachycardia syndrome, hypertension, diabetes), and inflammatory or pain syndromes (arthritis, fibromyalgia). Many of these studies are early-phase or small sample size, so it’s important not to overstate results. Yet, consistent themes are reduction in sympathetic overactivity, improvement in vagal markers (like HRV), reduction in inflammatory indicators, and patient-reported improvements in symptoms.
One specific device often referenced in aVNS research is the Nurosym wearable (by Parasym). Nurosym is a CE-marked auricular VNS device that resembles a small earpiece; it delivers controlled electrical pulses to the tragus area. Unlike some DIY stimulators, it’s been used in numerous clinical collaborations. In fact, Nurosym (and similar devices) have been or are being studied with institutions like UCLA, King’s College London, and Maastricht University in conditions ranging from chronic fatigue to stroke recovery. For example, researchers at King’s College Hospital are trialing an ear vagus stimulator in stroke patients undergoing rehabilitation, to see if stimulation during physical therapy can speed up motor recovery 48,49. (This approach builds on US studies where invasive VNS paired with rehab improved stroke outcomes – now we test if ear VNS can do the same without surgery.) At UCLA, studies are examining if daily aVNS can help patients with long COVID or postural tachycardia (POTS) by recalibrating autonomic function. And at Maastricht, as noted, trials have looked at cognitive enhancement and IBS. Nurosym itself is marketed as a general wellness device for stress, sleep, and focus, but importantly it is backed by ongoing research – making it one of the more validated options in the burgeoning wearable VNS market.
In summary, while large-scale Phase III trials are still needed in many areas, the evidence so far suggests that auricular VNS is a promising tool to influence the brain-body axis. It offers a kind of “digital drug” that can nudge the autonomic nervous system toward balance, with ripple effects on inflammation, mood, and organ function. The coming years should bring more clarity on which conditions benefit the most, optimal dosing regimens, and long-term effects of chronic use. But even the current data provide hope that stimulating your vagus nerve through your ear could become a commonplace, science-backed therapy for whole-body wellness.
Frequently Asked Questions
A: For most people, yes – it appears very safe. Unlike implanted VNS which requires surgery, transcutaneous aVNS is non-invasive. Reported side effects in studies are usually minor: slight skin irritation on the ear, tingling, or a pressure sensation during stimulation. A systematic review of taVNS safety found no serious adverse events across hundreds of patients, concluding that aVNS is a feasible and well-tolerated therapie 25. However, aVNS is not recommended for individuals with electrical implants like pacemakers or those with epilepsy unless under medical supervision, as the effects on seizure threshold are still being studied. Always start with low intensity if you’re new to aVNS, and consult a healthcare provider especially if you have underlying medical conditions.
A: This can vary by individual and condition. Some people notice an immediate calming effect (e.g. feeling more relaxed, breathing easier after a 15-minute session). For clinical outcomes, like improvements in depression or digestion, it often takes a few weeks of regular use. In the postpartum depression study mentioned, significant mood improvements accrued over 4–6 weeks of daily stimulation 34,35. In trials for pain or IBS, reductions in symptoms were seen after a few weeks of consistent daily sessions. Essentially, while acute physiological changes (heart rate, etc.) occur during each stimulation, the therapeutic benefits on complex symptoms likely require repeated stimulation over time – akin to physical therapy for your nervous system. Patience and consistency are key; many protocols suggest using the device daily for at least a month to gauge its benefits
A: Research is ongoing, but evidence exists for: depression and anxiety (especially hard-to-treat cases, as an adjunct to other treatments), PTSD, headaches (migraine and cluster), IBS and functional gut disorders, autoimmune conditions (rheumatoid arthritis, Crohn’s disease – vagal stimulation may reduce inflammatory flares), and post-stroke rehabilitation (to enhance motor recovery). People with chronic fatigue syndrome or long COVID have also reported improvements in energy and cognitive function anecdotally. Additionally, healthy individuals are using aVNS for stress reduction, better sleep, and focus. While it’s not a panacea, the vagus nerve’s broad role means stimulating it can have system-wide effects – from calming the mind to soothing the gut. It’s important to set realistic goals and use aVNS as a complement, not replacement, to standard medical care for any condition.
A: Anyone with a cardiac pacemaker, implanted defibrillator, or other electrical implant should not use electronic stimulators without medical approval – the electrical pulses could (in theory) interfere with such devices. Those with epilepsy should consult their neurologist; paradoxically, while VNS is an approved epilepsy treatment, any neuromodulation should be professionally guided in epilepsy due to the small risk of affecting seizure patterns. If you have low blood pressure or a history of fainting (vasovagal syncope), be cautious – vagus stimulation might trigger a faint in very susceptible individuals (although this is uncommon with gentle auricular pulses). Pregnant women should also seek medical advice before using aVNS, as strong vagal stimulation might theoretically affect uterine contractions (again, no direct evidence of harm, but caution is prudent). Finally, avoid placing electrodes on irritated or wounded skin on the ear. In general, if you have major medical issues, get a thumbs-up from your doctor first.
A: Absolutely. In fact, it’s often best used in combination with other approaches. For mental health conditions, aVNS can augment antidepressant medications or psychotherapy by putting the body in a calmer state more receptive to healing. In inflammatory or pain conditions, it can work alongside drugs (e.g. imagine using aVNS plus an anti-inflammatory medication to tackle rheumatoid arthritis from both angles). There are also intriguing combinations being studied: for instance, pairing aVNS with exposure therapy in PTSD, to help patients stay grounded during trauma processing; or with physical therapy in stroke rehab, to potentially accelerate neuroplasticity (the King’s College stroke trial is an example). No significant adverse interactions have been noted between aVNS and medications. The main consideration is to time things appropriately – e.g. do not use aVNS at the exact same moment as a transcranial magnetic stimulation (TMS) session or other electrotherapy, to avoid any interference (space them out by an hour or more). Otherwise, think of aVNS as a supportive modality that can synergize with lifestyle changes (exercise, diet), stress management, and standard medical treatments.
Conclusion: Why Understanding the Vagus Nerve Matters
The vagus nerve is a literal lifeline connecting brain to body, and an essential regulator of our physiological and emotional health. As science unravels the myriad ways vagal signals keep us balanced – from calming the heart, to digesting food, to toning down inflammation and anxiety – it becomes clear that nurturing one’s vagus nerve is pivotal for overall wellness. When the vagus is in harmony, we tend to feel grounded, resilient, and healthy. Conversely, when vagal tone is low or the nerve is thrown off-kilter, multiple systems can suffer. Fortunately, we live in an exciting time where ancient wisdom (like the benefits of deep breathing and meditation) converges with cutting-edge biomedical technology (like auricular VNS devices) to give us tools for enhancing vagal function.
For those struggling with stress-related ailments, depression, gut disorders, or autoimmune diseases, therapies targeting the vagus nerve offer a novel and promising avenue – often with few side effects. Even for those in good health, incorporating vagus-friendly practices (such as breathing exercises or cold finish showers) could boost your resilience in our stress-filled modern world. And if you seek more intensive help, clinically-tested options like Nurosym and other aVNS devices are increasingly accessible to consumers, bringing what used to be a specialized hospital therapy right to your home. Before long, stimulating your vagus nerve might be as commonplace as taking a daily supplement.
In summary, the humble vagus nerve carries immense influence over mind and body. By understanding its role and how to engage it, we gain a powerful lever to shift our physiology toward balance and healing. The emerging research is painting a hopeful picture: whether through a simple “Om” chant or a sophisticated medical device, tapping into the vagus nerve’s superhighway can lead to better health outcomes. The story of the vagus nerve exemplifies the intricate connection between the brain, body, and behavior – and it gives credence to the idea that by modulating our biology, we can profoundly affect our well-being. As research continues to evolve, the vagus nerve stands out as a key frontier in medicine, one that could unlock new treatments for some of our most challenging health issues. In the meantime, don’t hesitate to show your vagus nerve some love – your body and brain will thank you for it.
Der Artikel stellt in keiner Weise eine medizinische Beratung dar. Bitte konsultieren Sie einen zugelassenen Arzt, bevor Sie eine Behandlung beginnen. Diese Website kann Provisionen für die in diesem Artikel erwähnten Links oder Produkte erhalten.
References
Badran, B. W., Mithoefer, O. J., Summer, C. E., LaBate, N. T., Glusman, C. E., Badran, A. W., … & George, M. S. (2018). Short trains of transcutaneous auricular vagus nerve stimulation (taVNS) have parameterspecific effects on heart rate. Brain Stimulation, 11(4), 699–708. https://doi.org/10.1016/j.brs.2018.04.004
Berthoud, H. R., & Neuhuber, W. L. (2000). Functional and chemical anatomy of the afferent vagal system. Autonomic Neuroscience, 85(1–3), 1–17. https://doi.org/10.1016/S1566-0702(00)00215-0
Bonaz, B., Picq, C., Sinniger, V., Mayol, J. F., & Clarençon, D. (2013). Vagus nerve stimulation: from epilepsy to the cholinergic anti-inflammatory pathway. Neurogastroenterology & Motility, 25(3), 208–221. https://doi.org/10.1111/nmo.12076
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience, 9(1), 46–56. https://doi.org/10.1038/nrn2297
Frangos, E., Ellrich, J., & Komisaruk, B. R. (2015). Non-invasive access to the vagus nerve central projections via electrical stimulation of the external ear: fMRI evidence in humans. Brain Stimulation, 8(3), 624–636. https://doi.org/10.1016/j.brs.2014.11.018
Groves, D. A., & Brown, V. J. (2005). Vagal nerve stimulation: a review of its applications and potential mechanisms that mediate its clinical effects. Neuroscience & Biobehavioral Reviews, 29(3), 493–500. https://doi.org/10.1016/j.neubiorev.2005.01.004
Jacobs, H. I. L., Riphagen, J. M., Razat, C. M., Wiese, S., & Sack, A. T. (2015). Transcutaneous vagus nerve stimulation boosts associative memory in older individuals. Neurobiology of Aging, 36(5), 1860–1867. https://doi.org/10.1016/j.neurobiolaging.2015.02.023
Jerath, R., Edry, J. W., Barnes, V. A., & Jerath, V. (2006). Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Medical Hypotheses, 67(3), 566–571. https://doi.org/10.1016/j.mehy. 2006.02.042
Kaczmarczyk, R., Tejera, D., Simon, B. J., & Heneka, M. T. (2018). Microglia modulation through external vagus nerve stimulation in a murine model of Alzheimer’s disease. Journal of Neurochemistry, 146(1), 76– 85. https://doi.org/10.1111/jnc.14284
Porges, S. W. (2001). The polyvagal theory: phylogenetic substrates of a social nervous system. International Journal of Psychophysiology, 42(2), 123–146. https://doi.org/10.1016/S0167-8760(01)00162-3
Porges, S. W. (2009). The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system. Cleveland Clinic Journal of Medicine, 76(Suppl 2), S86–S90. https://doi.org/10.3949/ccjm. 76.s2.17
Tang, Y.-Y., Hölzel, B. K., & Posner, M. I. (2015). The neuroscience of mindfulness meditation: how the brain changes shape with practice. Nature Reviews Neuroscience, 16(4), 213–225. https://doi.org/10.1038/ nrn3916
Thayer, J. F., & Lane, R. D. (2000). A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders, 61(3), 201–216. https://doi.org/10.1016/ S0165-0327(00)00338-4
Yuan, H., & Silberstein, S. D. (2016). Vagus nerve and vagus nerve stimulation, a comprehensive review: Part II. Headache, 56(2), 259–266. https://doi.org/10.1111/head.12650
1, 12, 15 Vagus nerve stimulation: from epilepsy to the cholinergic anti-inflammatory pathway –
PubMed
https://pubmed.ncbi.nlm.nih.gov/23360102/
2 The inflammatory reflex – PubMed
https://pubmed.ncbi.nlm.nih.gov/12490958/
3, 16 Polyvagal theory – Wikipedia
https://en.wikipedia.org/wiki/Polyvagal_theory
4 Functional and chemical anatomy of the afferent vagal system – PubMed
https://pubmed.ncbi.nlm.nih.gov/11189015/
5 Auricular branch of vagus nerve – Wikipedia
https://en.wikipedia.org/wiki/Auricular_branch_of_vagus_nerve
6 Transcutaneous Auricular Vagus Nerve Stimulation – PubMed Central
https://pmc.ncbi.nlm.nih.gov/articles/PMC8192665/
7, 8 Non-invasive Access to the Vagus Nerve Central Projections via Electrical Stimulation of the External Ear: fMRI Evidence in Humans – PubMed
https://pubmed.ncbi.nlm.nih.gov/25573069/
9, 27 Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system – PubMed
https://pubmed.ncbi.nlm.nih.gov/16624497/
10, 11 Better insight into the vagus nerve’s link to brain | ScienceDaily
https://www.sciencedaily.com/releases/2022/07/220728134052.htm
13 A model of neurovisceral integration in emotion regulation and dysregulation – PubMed
https://pubmed.ncbi.nlm.nih.gov/11163422/
14 Heart rate variability is enhanced in controls but not maladaptive …
https://www.sciencedirect.com/science/article/abs/pii/S0167876015002159
17 The role of Epstein–Barr virus and the gut–brain axis – PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC11041741/
18, 19 Cytokine, Sickness Behavior, and Depression – PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC2740752/
20, 21 Microglia modulation through external vagus nerve stimulation in a murine model of Alzheimer’s disease – PubMed
https://pubmed.ncbi.nlm.nih.gov/29266221/
22, 24 Vagus Nerve and Vagus Nerve Stimulation, a Comprehensive Review: Part II – PubMed
https://pubmed.ncbi.nlm.nih.gov/26381725/
23 Vagus Nerve Stimulation (VNS): What It Is, Uses & Side Effects
https://my.clevelandclinic.org/health/treatments/17598-vagus-nerve-stimulation
25 Safety of transcutaneous auricular vagus nerve stimulation (taVNS)
https://www.nature.com/articles/s41598-022-25864-1
26, 41 Transcutaneous auricular vagus nerve stimulation and heart rate …
https://www.sciencedirect.com/science/article/abs/pii/S1566070221001247
28 Neurohemodynamic correlates of ‘OM’ chanting – LWW.com
https://journals.lww.com/ijoy/fulltext/2011/04010/neurohemodynamic_correlates_of__om__chanting__a.2.aspx
29, 30, 33 Does Dunking Your Head in Water Ease Anxiety? Ask This Professor’s Diving Mice | College and Graduate School of Arts and Sciences, University of Virginia
https://www.as.virginia.edu/does-dunking-your-head-water-ease-anxiety-ask-professors-diving-mice
31, 32 Face immersion increases vagal activity as assessed by heart rate variability – PubMed
https://pubmed.ncbi.nlm.nih.gov/9367278/
34, 35, 36, 37 Effect of transcutaneous auricular vagus nerve stimulation on major depressive disorder with peripartum onset: A multicenter, open-label, controlled proof-of-concept clinical trial (DELOS-1) – PubMed
https://pubmed.ncbi.nlm.nih.gov/35932937/
38, 39, 40 Transcutaneous vagus nerve stimulation boosts associative memory in older individuals – PubMed
https://pubmed.ncbi.nlm.nih.gov/25805212/
42, 43 Auricular Vagus Neuromodulation – A Systematic Review on Quality of Evidence and Clinical Effects | medRxiv
https://www.medrxiv.org/content/10.1101/2020.11.26.20239509v1.full-text
44 Transcutaneous Auricular Vagal Nerve Stimulation Is Effective for …
https://pubmed.ncbi.nlm.nih.gov/37787432/
45 Efficacy and Safety of Transcutaneous Auricular Vagus Nerve
https://journals.lww.com/ajg/fulltext/9900/efficacy_and_safety_of_transcutaneous_auricular.1490.aspx
46 Vagus nerve stimulation increases stomach-brain coupling via a …
https://www.brainstimjrnl.com/article/S1935-861X(22)00197-8/fulltext
47 Transcutaneous vagus nerve stimulation: a new strategy … – Frontiers
https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2024.1334887/full
48 49 Kings College trials stimulation therapy for stroke patients – BBC News
https://www.bbc.co.uk/news/articles/crmzyr7nx1lo



